Perimenopause & Mental Health
Perimenopause may start 10-15 years before the final menstrual period, the late 30s-early 40s for many. During this transition, women experience significant hormonal fluctuations that can profoundly affect their mental health. This can present initially as worsening of PMS, crying for no reason, free-floating anxiety, or thoughts of hopelessness or helplessness. These symptoms are not discussed as much as hot flashes or weight gain, but can be extremely disruptive to relationships and work performance. Understanding these hormonal changes can help women better manage their mental health during this transitional phase.
1. Estrogen Fluctuations can lead to unpredictable mood swings, anxiety, and depression because estrogen plays a crucial role in regulating neurotransmitters like serotonin and dopamine, which are essential for mood stability.
2. Progesterone Decline: Progesterone has a calming effect on the brain and helps promote sleep. Lower levels can lead to sleep disturbances, which can exacerbate mood issues.
3. Testosterone Decline can lead to reduced energy levels and decreased motivation, contributing to feelings of fatigue and low mood.
4. Thyroid Function may be altered with hormonal changes, which can influence mood and energy levels, leading to fatigue, depression, and cognitive difficulties, which can compound perimenopausal symptoms.
A word about PMDD: perimenstrual mood disorders (aka really bad PMS)
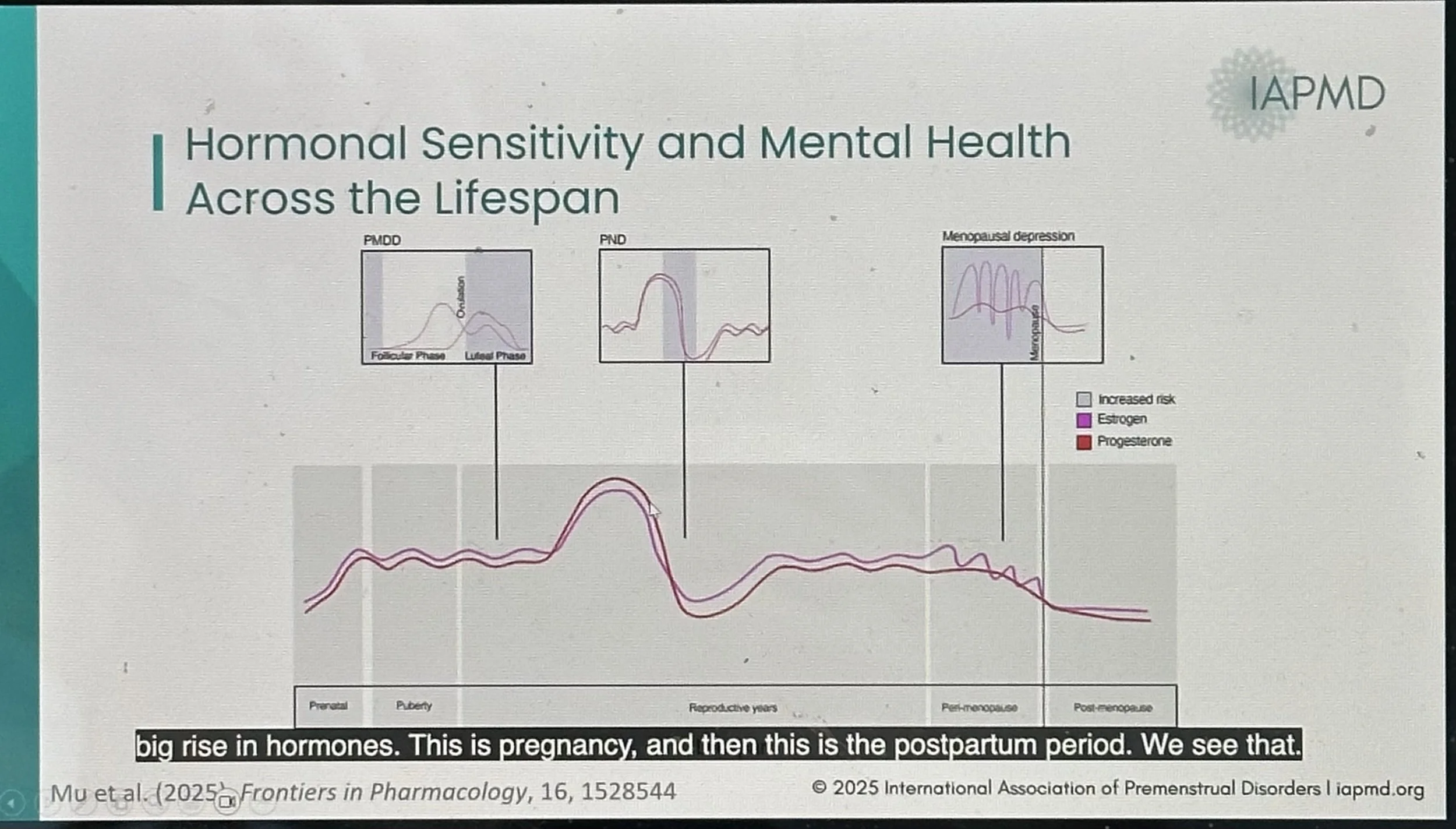
Some women are exquisitely sensitive to the hormonal (estradiol and/or progesterone) changes (increasing and/or decreasing) throughout the cycle (PMDD) and throughout the reproductive lifespan (perinatal, perimenopause). Perimenstrual, perinatal, and perimenopausal symptoms should be thought of as a continuum reflecting sensitivity to hormonal fluctuations throughout life.
For PMDD:
Cycle days ~4-10 are typically the least symptomatic, with increased symptoms in the luteal phase.
Distinct duration of symptoms (on/off) vs exacerbation of the underlying mental health condition, like depression or anxiety (on/worse).
Often misdiagnosed; can take up to 20 years for diagnosis.
Sufferers are at increased risk of work and personal relationship issues, sick leave, unemployment, and divorce. Perimenopause represents the highest risk period for suicidal ideation when women are 2x’s more likely to die of suicide.
People with PMDD may find worsening or lengthening of symptoms, which used to be predictable days before menses, now stretch to 2-3 weeks of the month. You can also continue to have “cyclical” mood changes when skipping menses.
Hormone levels are unhelpful:
These hormones may be changing at the same time, and frequently.
This is not a “hormone imbalance”; there is no such thing.
There are no “target levels” for treatment.
Mental health changes are common during perimenopause
Women are 2 -5 times more likely to experience depression, low mood, anxiety, mood swings, insomnia, and attention and concentration difficulties. This risk is increased for those during times of hormone fluctuation, like perimenstrually or perinatally.
Symptoms can be new or an exacerbation/recurrence of psychiatric issues experienced earlier in life and may include thoughts of self-harm.
Previous depression, anxiety, PMDD, ADHD, endometriosis, and PCOS can increase risk.
Risk also increased with the removal of ovaries and/or uterus and frequent hot flashes/night sweats, major life changes or stress, lack of social support, insomnia, poor nutrition, alcohol misuse, and lack of activity.
Nutrient deficiencies, though not directly related to hormone fluctuations, may be present and can exacerbate perimenopausal mental health symptoms and fatigue.
Not all mental health symptoms are due to hormonal fluctuations; as a corollary, not all mental health symptoms can be improved with hormone therapy. Even when hormonally-mediated, some may feel best with a combination of hormones + medications.
Treatment options and self-care strategies
A combination of treatments works best for most:
Psychotherapy, like Cognitive Behavioral Therapy, is a first-line treatment for depression and anxiety, improving mood and sleep. Often, 10-12 sessions are all that is required. Please see my list of therapy referrals here
Psychiatric Medications are effective for treating depression, anxiety, and hot flashes. Common options include bupropion, buspirone, escitalopram, sertraline, and desvenlafaxine. If a medication worked in the past, it may work now.
Hormone Therapy is not FDA-approved for pre-existing major depression or generalized anxiety disorders; rather, it can reduce depressive or anxious symptoms, improve mood, hot flashes, and sleep disturbance that are due to hormonal fluctuations.
Self-Care Strategies like exercise, sleep hygiene, mindfulness, stress reduction, and social support are crucial for supporting mental health.
Supplements are not considered first-line treatment, but may be helpful for mild symptoms or as an adjunct to hormone therapy. Few have evidence to support their use, and beware when combining with psychiatric medications*:
*St. John's Wort 300mg three times a day
Saffron 15mg twice a day
*SAM-e 800mg once or twice a day
Omega-3 fatty acids (EPA/DHA) 1000-2000mg per day
B vitamins, vitamin D, and iron if low or low normal levels
Specifically for sleep and/or anxiety: Kava, GABA, magnesium glycinate
When to seek help
Persistent feelings of sadness or hopelessness lasting over two weeks.
Loss of interest in activities you once enjoyed.
Anxiety that interferes with daily life.
Thoughts of self-harm.
Symptoms disrupting work, relationships, or quality of life
Self-screeners & tracking forms
For generalized depression, mood disorders & anxiety
Hormone cycle symptoms tracker if your symptoms are affected by your menstrual cycle.
Articles on the impact of female reproductive hormones & mental health
Perimenstrual Hormone Fluctuations & Suicide Risk: Current Psych Reports (2018)
Can Menopause Cause Depression? : Johns Hopkins
The Effects of Estrogen on Women’s Moods & Emotions: WebMD (2024)
Fear of Being Labeled Hysterical: 1 in 10 women experience suicidal thoughts due to perimenopause - The Independent (2021)
Resources for hormones & mental health support